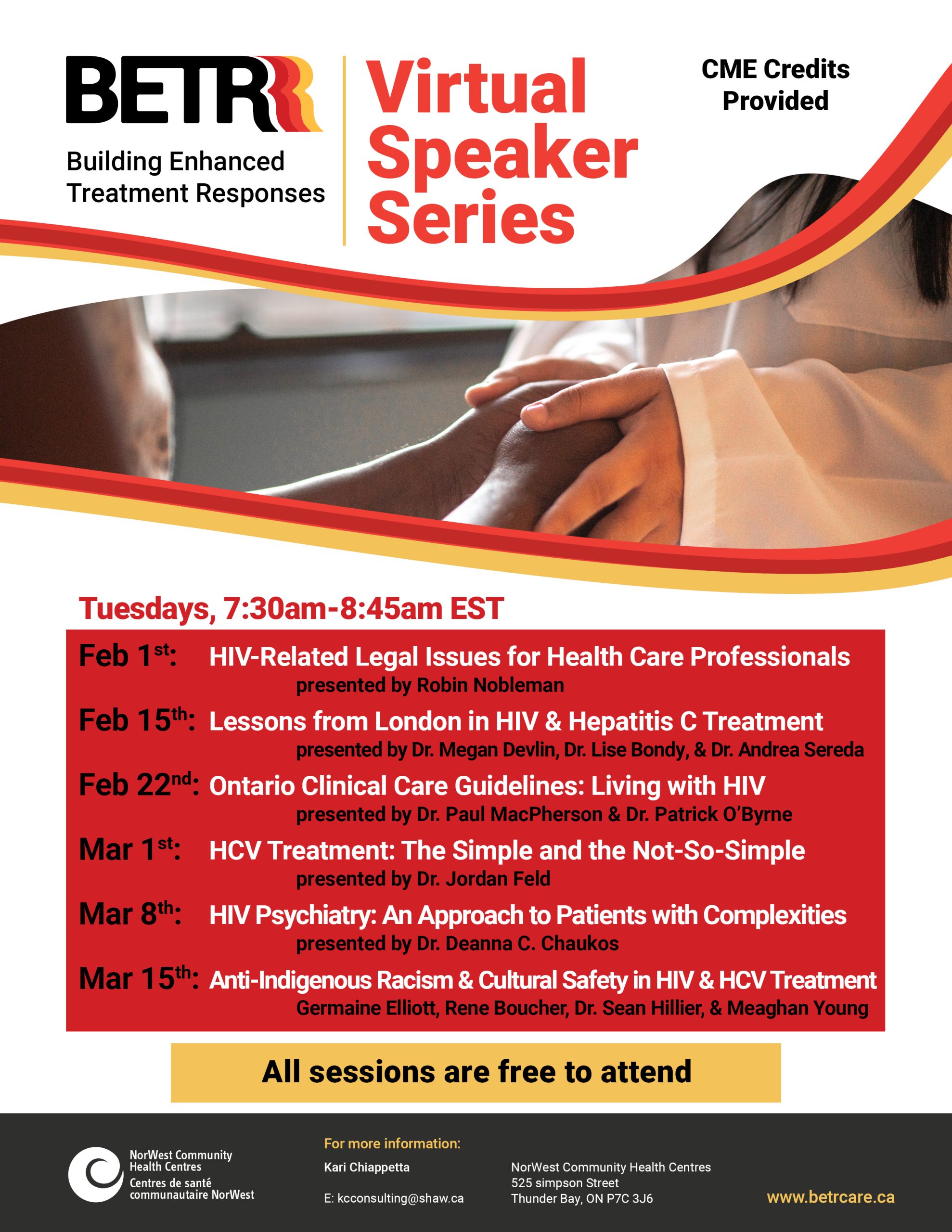
BETR Virtual Speaker Series
Click here to register
Schedule and Session Summaries
HIV-Related Legal Issues for Health Care Professional
Tuesday February 1, 2022, 7:30 am – 8:45 am EST
Robin Nobleman
The importance of a human rights and privacy focused approach to the provision of services for people living with HIV. Discussion of key legal issues facing people living with HIV, including the criminalization of HIV non-disclosure, and how the issues intersect with the provision of health services.
Robin Nobleman has been a Staff Lawyer at the HIV & AIDS Legal Clinic Ontario (HALCO) since 2017. Following her MSc in Health, Community and Development, she worked in health policy and front-line service provision in Canada and internationally. After graduating from Osgoode Hall Law School in 2015, she articled and practiced as a litigator at a leading labour and employment firm. Robin is now HALCO’s litigation lawyer; she represents people living with HIV, provides public legal education, and engages in law reform and public interest litigation. Robin’s practice includes health law, privacy, human rights, income security, and housing law. Robin also sits on the Board of Directors of the Wellesley Institute, a health equity think tank, and has taught Public Health Law as an Adjunct Professor at the University of Toronto’s Faculty of Law.
Lessons from London in HIV and Hepatitis C Treatment
Tuesday February 15, 2022, 7:30 am – 8:45 am EST
Providing Patient-Centered Care for Patients Living with HIV Who Also Inject Drugs
Dr. Megan Devlin
Learning objectives:
1. Review a case illustrating medical care for person who injects drugs recently diagnosed with HIV
2. Describe the current models of care used in London, Ontario to support patients living with HIV with substance use history and / or unstable housing
3. Provide useful advice from nursing and outreach workers on providing supportive care for these patients
4. Discuss use of pre-exposure prophylaxis to prevent HIV in patients who inject drugs
Dr. Megan Devlin completed her medical school training at the Royal College of Surgeons in Ireland. She completed her residency in Internal Medicine and Infectious Diseases at the University of Toronto. She joined the Faculty of Medicine at Western University as an assistant professor in 2018. She currently specializes in providing HIV care to vulnerable populations, including people who inject drugs. She is the medical director for the MyCare Program which provides care to London’s most vulnerable patients living with HIV.
Hep C Treatment in People Who Use Drugs
Dr. Lise Bondy
Learning objectives:
1. Discuss the benefits of treating hepatitis C in people who use drugs
2. Address challenges in treating hepatitis C in people who use drugs
3. Review data on re-infection with hepatitis C in people who use drugs
Dr. Lise Bondy graduated from medical school at the University of British Columbia. She completed her internal medicine and infectious diseases training at the University of Toronto, then completed fellowship training in Hepatology at the Toronto Western Hospital Liver Centre. She is currently an Assistant Professor in the Division of Infectious Diseases at Western University. Her clinical interests include viral hepatitis, HIV and general infectious diseases. She works in the hepatitis C program at the London Intercommunity Health Centre and as an ID consultant for the Elgin Middlesex Detention Centre.
Safer Supply and the Impact That Has on People Living with HIV and Preventing Transmission
Dr. Andrea Sereda
Learning objectives:
1. Recognize potential harms to people who use the fentanyl street supply
2. Identify patients who may benefit from Safe Supply
3. Understand how Safe Supply can support HIV and HCV care, and apply this knowledge to their own patients
Dr. Andrea Sereda is a family physician working at the London Intercommunity Health Centre, where she focuses her practice on people who use drugs, people living in homelessness, and women involved in the survival sex trade. Dr. Sereda provides care in a traditional office setting, but also through street outreach medicine; going to where people are at in shelters, encampments or anything in between. She is an avid harm reductionist, and is the lead physician for the LIHC Safe Opioid Supply program, which is currently the longest running SOS program in Canada.
Ontario Clinical Care Guidelines: for Adults and Adolescents Living with HIV in Ontario, Canada
Tuesday February 22, 2022, 7:30 am- 8:45 am EST
Dr. Paul MacPherson & Dr. Patrick O’Byrne
The Ontario Clinical Care guidelines were developed in 2017 to support primary care providers who are not familiar with providing HIV care to adults and adolescents in Ontario and to optimize clinical management of HIV infection across the province.
The guidelines set out evidence-based practices to help engage people with HIV in care in a timely way, retain them in care over time, address challenges that may cause them to fall out of care, assess them for relevant health issues and monitor all aspects of their health. They use a “patient journey” approach, beginning with diagnosis and then following the patient from the initial assessment or first visit(s), to initiation of treatment and ongoing care and support. They focus on the person’s history and life course, include strategies to reduce/manage co-infections and co-morbidities, provide recommendations on ongoing access to ART across the continuum of care to improve overall quality of life.
For people living with HIV, the guidelines clarify what they should expect from their providers. For health care providers, the guidelines set out expected assessments, tests and investigations as well as their recommended frequency. They include practical checklists that can be used in real-world health settings to ensure people with HIV receive comprehensive assessments.
Dr. Paul MacPherson is an Associate Professor of Medicine at the University of Ottawa with cross appointments in the Dept of Biochemistry, Microbiology and Immunology and in the School of Epidemiology and Public Health. He is a specialist in infectious diseases at the Ottawa Hospital, and a clinician-scientist at the Ottawa Hospital Research Institute. Dr MacPherson obtained his PhD from the University of California at Berkeley in 1991 and his MD from McMaster University in 1998. He completed his residency in internal medicine at the University of Toronto and subspecialty training in infectious diseases at the University of Ottawa. He has an active medical practice with a focus on HIV and other sexually transmitted infections, and has 20 years’ experience treating individuals with HIV infection.
Patrick O’Byrne RN-EC PhD is a Full Professor of Nursing and a licensed Nurse Practitioner. Dr. O’Byrne’s research and clinical work focus on the prevention, diagnosis, and management of sexually transmitted infections, including HIV. Dr. O’Byrne operates the PrEP-RN clinic in Ottawa and GetaKit for HIV self-testing in Ontario.
HCV Treatment: The Simple and The Not-So-Simple
Tuesday March 1, 2022, 7:30 am – 8:45 am
Dr. Jordan Feld
Learning Objectives:
1. Incorporation of simplified diagnosis and treatment paradigms for management of HCV
2. Identifying and overcoming challenging HCV treatment scenarios: severe liver disease and/or external factors including active substance use
Dr. Jordan Feld trained in GI and Hepatology at the University of Toronto and did post-doctoral training in the Liver Diseases Branch at the National Institutes of Health in laboratory and clinical research in viral hepatitis. After completing a Masters in Public Health at the Johns Hopkins Bloomberg School of Public Health, he returned to Toronto where holds the R. Phelan Chair in Translational Liver Research as a clinician-scientist at the Toronto Centre for Liver Disease in the Toronto General Hospital where he now leads a large clinical and translational research program focused primarily on viral hepatitis.
HIV Psychiatry: An Approach to Patients with Medical, Psychiatric and Psychosocial Complexity
Tuesday March 8, 2022, 7:30 am – 8:45 am EST
Dr. Deanna C. Chaukos
Learning Objectives:
1. Learn about the field of HIV Psychiatry, including the syndemics of HIV, mental illness and substance use, and compound impact of ACE (adverse childhood experiences) and other psychosocial barriers to health.
2. Identify important components of a psychiatric assessment, especially as it applies to patients living with HIV, recognizing that an approach to ambiguity is important.
3. Appreciate different skills to approach complexity, including the importance of collaboration across medical and community settings.
Dr. Deanna Chaukos is a Consultation/Liaison psychiatrist at Mount Sinai Hospital, and assistant professor at the University of Toronto Temerty Faculty of Medicine. Her clinical expertise includes care of patients with complex medical and psychiatric concerns, with an emphasis on Geriatrics and HIV psychiatry. She is the Associate Program Director for the University of Toronto Psychiatry Residency. She is involved in education innovation in HIV Psychiatry, including developing educational opportunities for mental health community workers that bridge hospital and community settings. She completed her MD at the University of Toronto Faculty of Medicine, residency in adult psychiatry at Harvard/ Massachusetts General Hospital and McLean Hospital, and fellowship in Consultation Liaison psychiatry at Massachusetts General Hospital.
Addressing Anti-Indigenous Racism & Providing Cultural Safety in Indigenous HIV & HCV Treatment
Tuesday March 15, 2022, 7:30 am – 8:45 am
Germaine Elliott, Rene Boucher, Dr. Sean Hillier, & Meaghan Young
This session is focused on 3 main areas as it relates to HIV and HCV Treatment for Indigenous peoples, these are:
1. Overview of Indigenous people’s experiences with discrimination as it relates to accessing healthcare services for HIV treatment. An overview of the data available through the Ontario Cohort Study will be provided.
2. an example will be provided of the work happening in Simcoe Muskoka to address anti-Indigenous racism in healthcare more broadly. Our goal is that this will help healthcare providers and allied health to have a better understanding of some tangible steps that they can take to inform their practice and the systems they work in.
3. a presentation by Oahas looking at stigma and how we approach providing support to individuals who have been diagnosis with HIV and HCV through a cultural safety lens.
Germaine Elliott is the Executive Director of Mamaway Wiidokdaadwin.
Rene Boucher is a Community Prevention Worker at Ontario Aboriginal HIV/AIDS Strategy (OAHAS).
Dr. Sean Hillier is an assistant professor at the School of Health Policy & Management & Special Advisor to the Dean on Indigenous Resurgence in the Faculty of Health at York University. He also is the Chair of the Indigenous Council at York and is Co-Chair of the Working Group on Anti-Black and Anti-Indigenous racism in the Faculty of Health.
Meaghan Young is the Executive Director of Ontario Aboriginal HIV/AIDS Strategy (OAHAS).
For more information on any of these sessions, please contact Kari Chiappetta at kcconsulting@shaw.ca.
